Why COVID-19 has spread faster than SARS
New research indicates that the virus that causes COVID-19 was more infectious than SARS when it emerged in Wuhan.
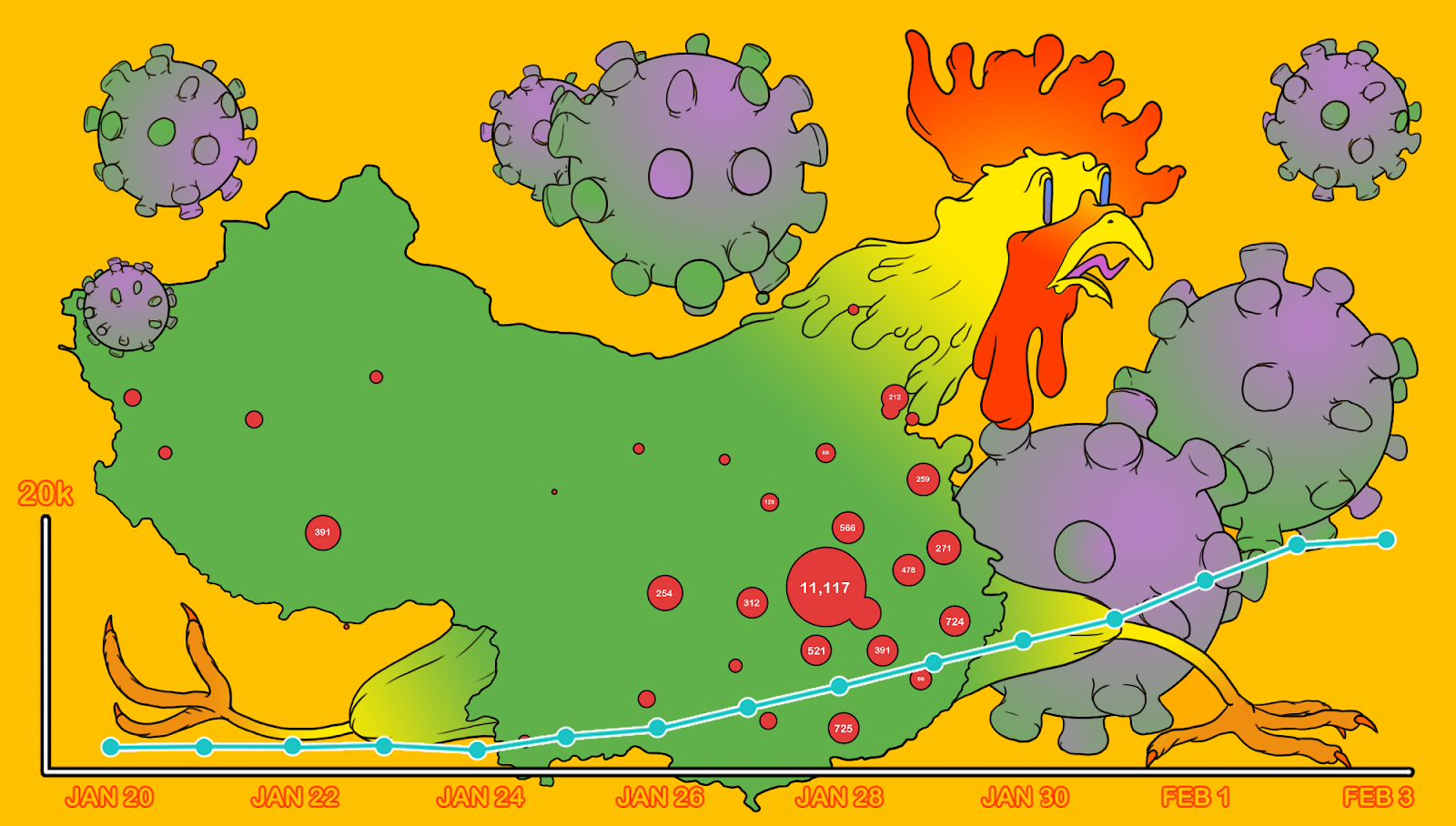
The China Project illustration by Derek Zheng, originally for our February 3 coronavirus update when, we noted, “it feels like the entire world is preparing for a pandemic.”
New research indicates that the virus that causes COVID-19 was more infectious than SARS when it emerged in Wuhan. While this does not sound surprising, given that COVID-19 has become a global pandemic, it does, significantly, contradict earlier research. Bloomberg reports:
Each person infected early in the epidemic in Wuhan probably passed the virus to an average of 5.7 other people, according to a mathematical analysis from Los Alamos National Laboratory. That’s more than twice what the World Health Organization and other public health authorities reported in February.
The 5.7 number refers to the R0 — pronounced R-naught — or the reproduction number of viruses, which is an approximation of the average number of people who will catch the disease from a single infected person. Early assessments of the R0 of the virus that causes COVID-19 had a wide range, but as summarized in late January by Ed Yong at The Atlantic, most put the number between 2 and 3. Yong used the example of SARS to explain what R0 means:
R0 is not some magical, immutable property of the virus itself. It depends on how likely someone is to be infected after contact with an infectious person, and how often such contact occurs—and these quantities are also affected by how societies deal with a virus. When SARS first emerged, transmission dynamics played out very differently in China and Canada, which is why the virus’s R0 values cover a wide range, from 2 to 5.
The Los Alamos team gives a caveat that “the lack of awareness of this new pathogen and the Lunar New Year travel and gathering in early and mid-January 2020 might or might not play a role in the high R0.” But its model estimates that by the time of the lockdown of Wuhan, on January 23, about 18,700 people had become infected — more than 30 times the official count of only 550 cases.
If the base transmission rate of COVID-19 is indeed so high, that would have significant implications for how soon any country can ease social distancing, and how long it will take to fully kill the virus and reach “herd immunity” in any population. The researchers write:
…the threshold for combined vaccine efficacy and herd immunity needed for disease extinction is calculated as 1 – 1/R0. At R0 = 2.2, this threshold is only 55%. But at R0 = 5.7, this threshold rises to 82% (i.e., >82% of the population has to be immune, through either vaccination or prior infection, to achieve herd immunity to stop transmission)…
Results show that quarantine and contact tracing of symptomatic persons can be effective when the fraction of unidentified persons is low. However, when 20% of transmission is driven by unidentified infected persons, high levels of social distancing efforts will be needed to contain the virus.
Other medical clues about the high contagiousness of COVID-19, and how it compares with SARS:
- A third of coronavirus cases may be ‘silent carriers,’ classified Chinese data suggests / SCMP
- Coronavirus may be most infectious when symptoms are mildest, small study finds / Live Science
-
What we know so far about SARS-CoV-2 / The Atlantic
“When SARS-classic first made this leap [from animal to human], a brief period of mutation was necessary for it to recognize [the target protein on human cells] well. But SARS-CoV-2 could do that from day one.” - Compare: 2003 SARS pandemic versus 2020 COVID-19 pandemic / BioSpace
Once SARS jumped to humans, it was transmitted from person to person. It is most virulent during the second week of infection when virus excretions through the mucus and stool peak.
With SARS, most human-to-human infections occurred in health care settings that lacked robust infection control procedures. When infection control practices were implemented, the outbreak ended.





